About
LEARN MORE ABOUT THE Event Event
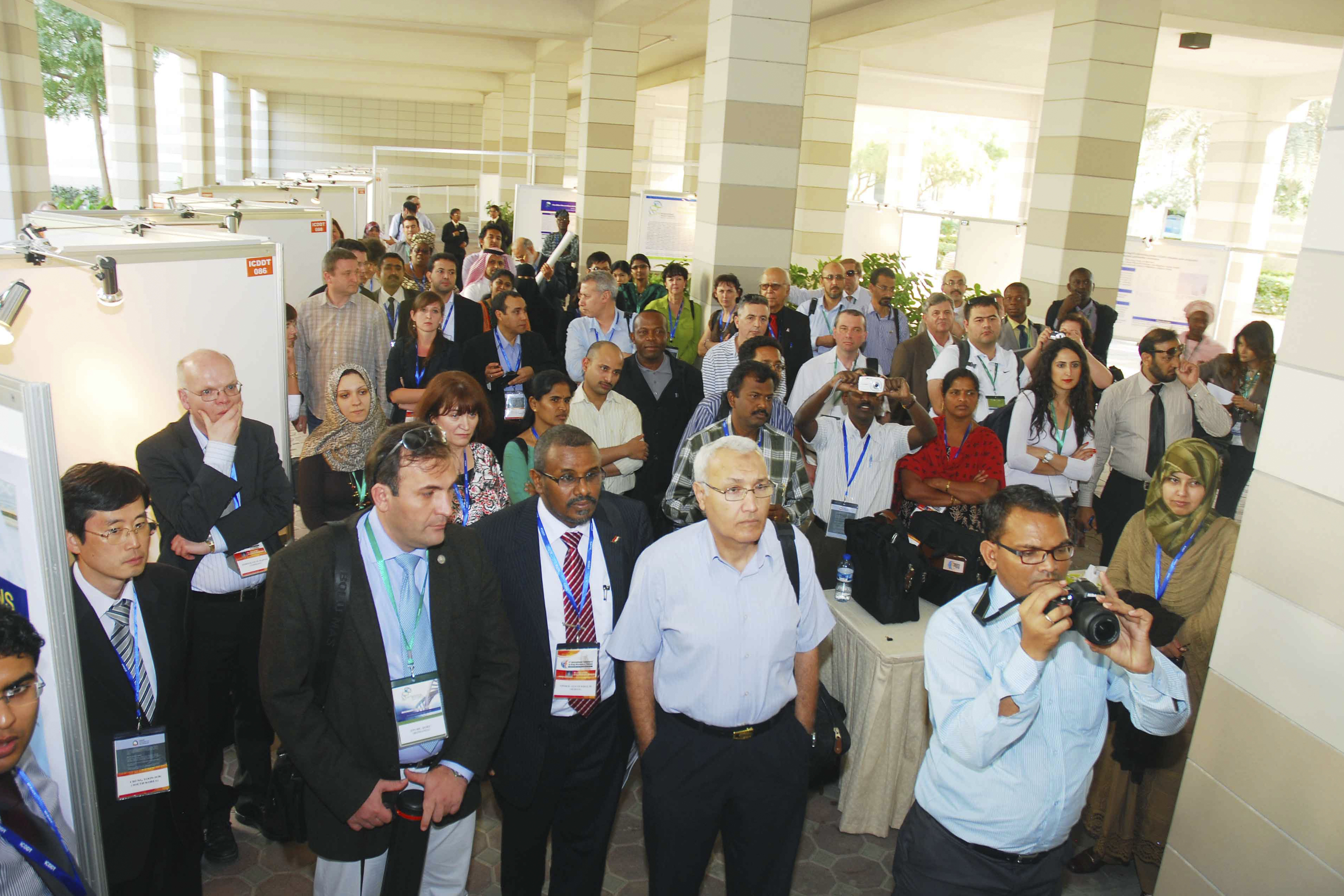
The International Medicine and Biosciences Conference 2025 (TIMBC 2025) is being organised by Eureka Science at Zayed University, Academic City, Dubai, UAE. This conference will be unique in bringing state-of-the-art in the fields of medicine and Biosciences closer to the doorstep of pharmaceutical scientists, internists and primary care physicians from all over the world. Zayed University, Dubai is located in the heart of the city, thereby providing the attendees of the conference with exciting opportunities for innumerable leisure activities.
The International Medicine and Biosciences Conference 2025 (TIMBC 2025), being the most innovative event, aims to provide an open and stimulating scientific and cultural exchange that will allow all the participants to share their experiences, foster collaborations across industry and academia, and evaluate emerging technologies across the globe.
As the previous conferences held in Dubai in February 2008, 2010, 2011, 2012, 2013, 2014 and 2016 (where many Nobel Laureates participated) had met with great success, the TIMBC 2025 is also augured to be a mega event with a series of exclusive talks to be delivered over a diverse range of thematic sessions along with poster presentations and an associated commercial exhibition.
TIMBC 2025 will be held at Zayed University, Dubai, which is located in the heart of the city, thereby providing the attendees of the conference with exciting opportunities for innumerable leisure activities.
WELCOME NOTE
The International Medicine and Biosciences Conference 2025, scheduled to be held from 6th - 8th November 2025 will bring together the world's leading scientists in the field of medicine and biosciences to discuss their latest research in the exciting setting of sunny Dubai. The conference should provide an occasion for the participating scientists not only to present their research and interact with eminent colleagues but also to enjoy the magical environment of the rich Arabian traditions and culinary delights of Dubai.